As COVID-19 vaccination programs are rolled out across the world, there have been increasing concerns regarding the lower uptake of vaccinations amongst minority groups. This concern was initially raised late last year, with several studies showing higher vaccine hesitancy amongst minority populations.
For example, a rapid national assessment in the United States1 found that Black and Hispanic individuals showed high rates of vaccine hesitation, at 34% and 29%, respectively. This was mirrored by a study published in The British Medical Journal in December 2020,2 which showed that vaccine hesitancy was higher amongst minority populations—specifically, Black, Bangladeshi, and Pakistani communities—than those from a white ethnic background.
Unfortunately, this hesitancy has translated into a worrying reality. Emerging data show that ethnic and racial minorities are being vaccinated at lower rates, even when controlling for unequal access to vaccinations.3 By March 11, in the U.K., 90.2% of all those over the age of 70 had received at least one dose of the COVID-19 vaccine, but for several groups in this age range, the rate of vaccination was much lower, as summarized in the figure below from the Office for National Statistics.4 The groups where uptake was the lowest were Black African and Black Caribbean (58.8% and 68.7% respectively), followed by people from Bangladeshi (72.7%) and Pakistani (74.0%) backgrounds.
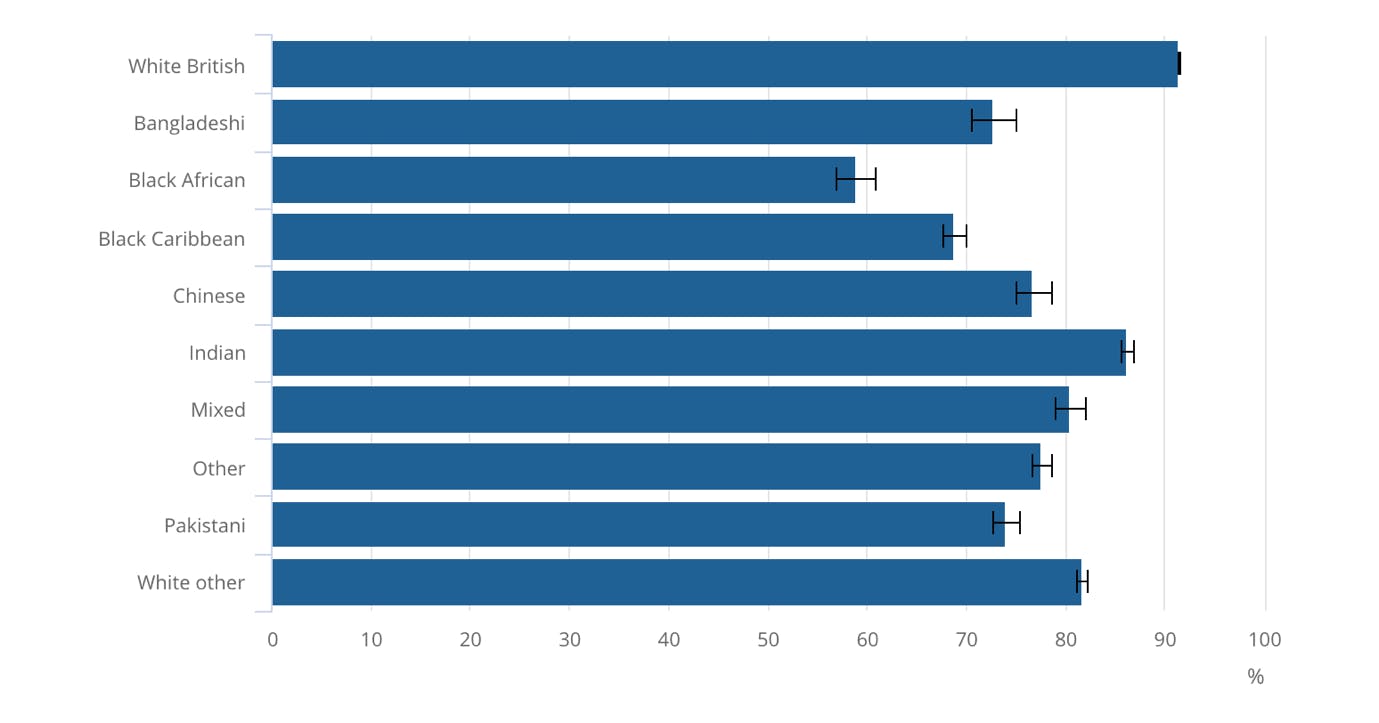
Figure 1: Vaccination rates of adults aged 70 years or over, by self-reported ethnic group, 8 December 2020 to 11 March 2021, England, ONS report 4
From popular culture to corporate boardrooms to politics, there has been increasing acknowledgment that minority representation is an extremely powerful tool to encourage and inspire others from the same background. And the evidence in a number of the fields mentioned above is robust. In the world of media and communications, it has been shown that increased visibility of minorities improves self-perception of minority identity and belief in the capabilities of minority people.5 The OECD has also stated that having strong and visible role models from minority populations encourages young people from the same background to achieve success in their education, and in the labor market more broadly.6
The evidence is clear that, in many cases, seeing really is believing. But what about in medicine? More specifically, when minority-identifying patients speak with and are vaccinated by doctors from minority populations, or they hear and see such physicians talking about vaccinations on the radio or television, what influence could this have on their likelihood of receiving a COVID-19 vaccine?
A look at the evidence
A working paper from the Stanford Institute for Economic Policy Research7 randomly assigned Black men to treatment by either Black or non-Black medical doctors. They measured their decisions about cardiovascular screening and the flu vaccine before and after meeting their assigned doctor.
The researchers found that Black men were much more likely to opt in to both interventions after meeting a doctor of the same race, and that this effect was most pronounced in those who did not routinely seek medical care and those who self-reported distrust in the medical system. Specifically, Black patients were 10% more likely to agree to receive the flu shot when they saw a Black doctor compared to those who were assigned a non-Black doctor.
More broadly, this concept is often termed patient-provider concordance (or patient-physician concordance) and refers to the influence of shared characteristics between patient and physician (including gender, race, socioeconomic status, and so on) on the patient’s overall treatment and healthcare utilization. Although initial reviews in the early 2000s were inconclusive,8 in recent years, higher-powered studies with larger sample sizes and randomized designs have shown that in fact, racial concordance is associated with significantly better health outcomes.
For example, a large study of over 100,000 individuals9 surveyed the race/ethnicity of patients as well as that of their physician, and also asked them about their satisfaction and experience with their physician (on a scale known as the Press Ganey scale). Although gender concordance did not make a significant difference on the Press Ganey Scale, patients with a physician of the same race had Press-Ganey scores that were more than 10% higher.
Similarly, a review of the literature in this area10 found that concordant patient-physician pairs were likely to have better communication, better partnership building, more information sharing, and longer visits. These patients were also more likely to agree to therapy when it was suggested by their physician.11
The factors that contribute to this are not well understood, but may include cultural competence and confidence (which can be taught)12 as well as less tangible factors, such as synchrony in non-verbal communication.13
Where does this leave us?
This article is not advocating that we match every patient with a physician of the same race. Not only would this be very difficult pragmatically14 and ethically15 (especially in defining what factors it is reasonable to seek concordance on), it is not applicable in all settings, nor is it a stable long-term solution. However, the truth remains that patients tend to listen more to, and have more positive clinical communications with, physicians of the same background.
In the short term, this can be harnessed in the communication of vaccine-related information. Having physicians who represent ethnic minorities talking to people about the vaccine, being shown on television, and heard on the radio talking about the importance of vaccination is likely to be of significant value.
In the long term, it shows us that there are factors, many of which are likely teachable and transferable, that can help all physicians become more adept at communicating with others, and in particular, with minority populations.
But for now, it is absolutely necessary to ensure that minority physicians are heard and seen, for they may hold the key to bridging the gap in vaccination rates.
References
- Khubchandani, J., et al., COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. Journal of Community Health, 2021. 46(2): p. 270-277.
- Razai, M.S., et al., Covid-19 vaccine hesitancy among ethnic minority groups. Bmj, 2021. 372: p. n513.
- Rubin, E.J., et al., Audio Interview: Delivering Covid-19 Vaccines to Minority Communities. New England Journal of Medicine, 2021. 384(13): p. e60.
- Statistics, O.f.N., Coronavirus and vaccination rates in people aged 70 years and over by socio-demographic characteristic, England: 8 December 2020 to 11 March 2021, O.f.N. Statistics, Editor. 2021: ons.gov.uk.
- Mahtani, M., Representing minorities: Canadian media and minority identities. Canadian Ethnic Studies Journal, 2001. 33: p. 99+.
- Froy, F.a.L.P., “Ensuring Labour Market Success for Ethnic Minority and Immigrant Youth. OECD Local Economic and Employment Development (LEED) Working Papers, 2011. 2011/09,.
- Alsan, M., O. Garrick, and G. Graziani, Does Diversity Matter for Health? Experimental Evidence from Oakland. American Economic Review, 2019. 109(12): p. 4071-4111.
- Meghani, S.H., et al., Patient-provider race-concordance: does it matter in improving minority patients’ health outcomes? Ethn Health, 2009. 14(1): p. 107-30.
- Takeshita, J., et al., Association of Racial/Ethnic and Gender Concordance Between Patients and Physicians With Patient Experience Ratings. JAMA Netw Open, 2020. 3(11): p. e2024583.
- Shen, M.J., et al., The Effects of Race and Racial Concordance on Patient-Physician Communication: A Systematic Review of the Literature. J Racial Ethn Health Disparities, 2018. 5(1): p. 117-140.
- Saha, S. and M.C. Beach, Impact of Physician Race on Patient Decision-Making and Ratings of Physicians: a Randomized Experiment Using Video Vignettes. J Gen Intern Med, 2020. 35(4): p. 1084-1091.
- Schinkel, S., et al., Enhancing Health Communication Outcomes Among Ethnic Minority Patients: The Effects of the Match Between Participation Preferences and Perceptions and Doctor–Patient Concordance. Journal of Health Communication, 2016. 21(12): p. 1251-1259.
- Hamel, L.M., et al., Nonverbal synchrony as a behavioural marker of patient and physician race-related attitudes and a predictor of outcomes in oncology interactions: protocol for a secondary analysis of video-recorded cancer treatment discussions. BMJ Open, 2018. 8(12): p. e023648.
- Turley, M., et al., The Feasibility of Automating Assessment of Concordance Between Advance Care Preferences and Care Received Near the End of Life. Jt Comm J Qual Patient Saf, 2019. 45(2): p. 123-130.
- Blythe, J.A. and F.A. Curlin, How Should Physicians Respond to Patient Requests for Religious Concordance? AMA J Ethics, 2019. 21(6): p. E485-492.
